Best Practices Guide: Enhancing Rural Hospital Care with AI-Powered Virtual Monitoring
AI-powered virtual monitoring is helping rural hospitals achieve 70–90% reductions in patient falls while covering 95% of high-risk patients instead of just 5–10%. With new federal funding through the Rural Health Transformation Fund, this guide shows how AI acts as a force multiplier—one observer can now monitor dozens of patients, extending care capacity without burdening lean staff in resource-constrained settings.

Best Practices Guide: Enhancing Rural Hospital Care with AI-Powered Virtual Monitoring
Rural hospitals are vital to the communities they serve, operating with limited staff, constrained resources, and technology that often complicates rather than facilitates care delivery. Virtual monitoring, enhanced by artificial intelligence (AI) and computer vision, is emerging as a scalable solution to extend care without burdening frontline teams.
This guide draws on lessons from rural hospitals that have adopted AI-enabled monitoring platforms to reduce falls and deliver more responsive patient care. With the One Big Beautiful Bill Act (OBBBA) budget and the new Rural Health Transformation Fund highlighting the need for durable strategies, AI can be part of the foundation rural hospitals use to set themselves up for long-term success.
Starting with a Perpetual Problem – Fall Prevention
Falls remain a critical concern nationwide, reflecting the lack of personnel capacity that significantly impacts the rural hospital setting. The lessons applied here thus have broader implications for successful AI programs.
Some rural hospitals using virtual monitoring have achieved 70–90% reductions in fall rates among monitored patients. Yet, due to costs, coverage was often limited to 5–10% of high-risk patients, making macro-level impact elusive.
Expanding requires three elements, and their principles apply well beyond fall prevention. Together, they lay the foundation for a broader category of enhanced safety and care programs that technology, particularly AI, is equipped to support.
- Leadership and buy-in across levels - Programs must matter to both leadership and frontline staff to drive systemic change.
- Simplicity - Technology must work reliably without requiring nurses and clinicians to become IT experts.
- Technology (AI) must be a multiplier - Systems must enhance capacity, not merely relocate workload.
With these strategies, some hospitals have increased coverage to more than 95% of high-risk fall patients, who often represent nearly half of inpatients, to create strategic impact.
Leadership and Buy-In
A turning point for one rural hospital occurred when the chief nursing officer found her own mother, who was at high risk of falling, wandering the halls without supervision. This incident highlighted significant gaps in the hospital’s patient monitoring procedures.
Elsewhere, a caregiver shared, “I made sure my mom came here because I knew someone would be watching.”
Personal stories like these turn adoption into lasting commitment and reflect that both leadership and frontline teams are necessary to unlock adoption.
Simplified, Scalable Technology
Rural hospitals often contend with complex telehealth setups and unreliable equipment. Even when vendors cite 99.9% uptime, inconsistent last-mile issues (e.g., poor Wi-Fi) can erode trust. Bridging the gap between technical metrics and frontline experience is essential.
Technology as a Multiplier of Capacity
While many solutions are promising, few are cost-effective enough to drive lasting change. AI is the first technology that can see and hear in patient rooms, letting one observer monitor all high-risk patients instead of just a few. Technology should expand capabilities, not just be another layer on existing staff.
Importantly, recent research shows rural hospitals adopt AI at lower rates compared to their urban peers—yet the smaller size and tighter resource constraints in rural facilities mean AI can deliver greater and more immediate impact in these settings. When technology extends a nurse’s attention across dozens of patients, it can transform outcomes where every staff member already wears multiple hats.
A Foundation for the Future
The same systems protecting vulnerable patients are also supporting caregivers. Beyond falls, AI-powered monitoring can help:
● Proactive detection of pressure injuries
● Alerts for changes in patient mobility
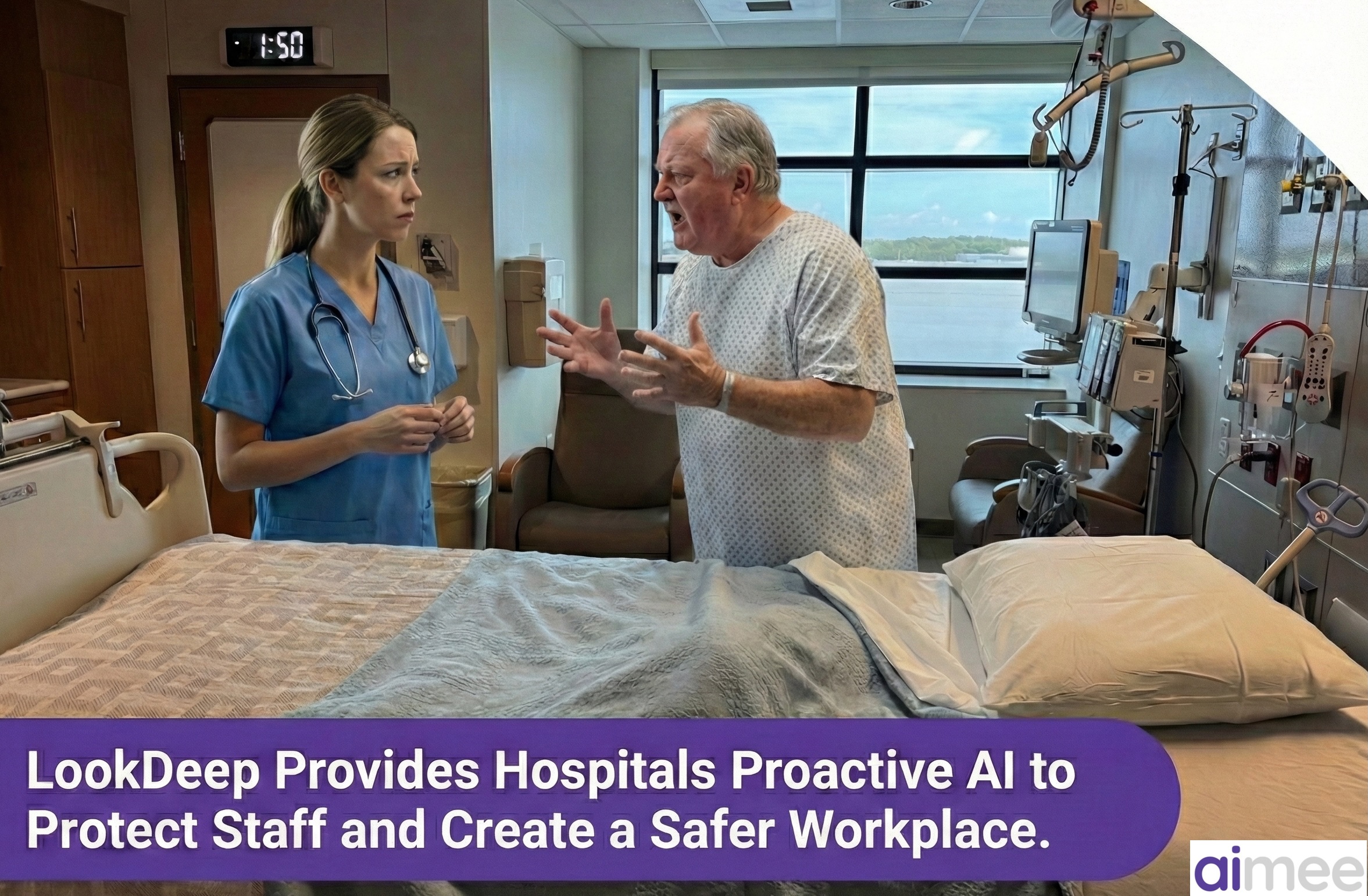
● Helping prevent workplace violence
● Patient companions to help with simple needs, like discussing meal choices
One doctor recalled ordering telemetry just to get extra attention for frail patients. Now, continuous monitoring provides that vigilance by design, without extra equipment or workarounds.
Rural hospitals require AI solutions that are tailored to their unique reality – smaller settings where everyone contributes and work is done by individuals, not large departments. That means less “smart” technology that just adds more dashboards or screens, and more tools that stand beside your staff – supporting care directly in the room, helping them do the work for patients instead of just documenting it. AI that works this way can make a hospital feel like it has more hands on deck, giving nurses and doctors the backup they need to care for patients the way they want to – together, all hands in.